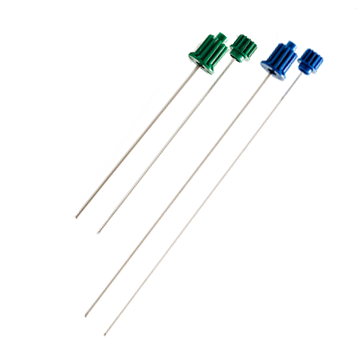
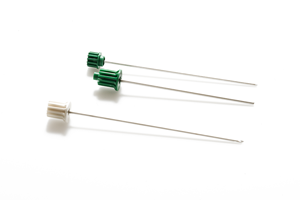
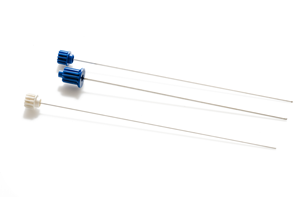
Coaxial bone biopsy system
The Bonopty® 14G system for bone biopsies has been a success since it first reached the market. Today, Bonopty® 14G exists in three lengths, all to perfectly match your various needs.
- Gain access into the bone, even through thick cortical bone
- Coaxial system facilitates multiple sampling, or treatment of lesions
- Achieve excellent core samples with few crush artifacts
- Successfully sample somewhat sclerotic lesions
- A variety of lenghts enhance perfect match for every procedure